Abstract
Introduction: Real world outcome data for Waldenstrom Macroglobulinemia (WM) is limited due to relatively rare and indolent nature of this B cell Non-Hodgkin lymhoplasmacytic lymphoma. In this retrospective analysis, we utilized National Cancer Data Base (NCDB) to identify variables contributing to the overall survival (OS) of over 14,000 WM patients treated at Commission on Cancer (CoC)-accredited cancer centers across USA.
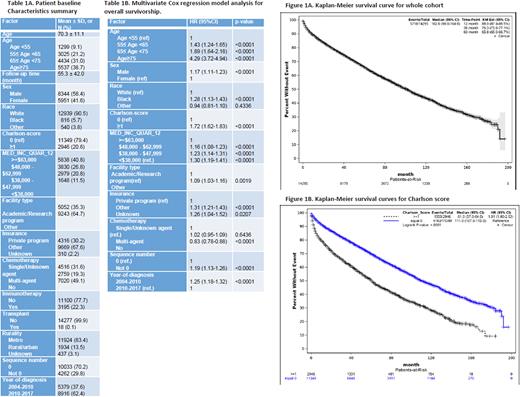
Methods: From NCDB, 14,295 WM patients diagnosed and treated during 2004-2017 were identified and included in the analysis after excluding entries with missing relevant values. For OS, univariate analysis was used first to summarize and assess the potential survival factors individually, and multivariate Cox regression analysis with backward elimination was utilized to identify the most important survival factors. In addition, Kaplan-Meier survival curves of patient cohort were also produced for OS. SAS version 9.4 was used to analyze the data.
Results: The baseline characteristics of the patients are shown in Table 1A. Multivariate Cox regression analysis with backward elimination method revealed that there were 10 significant independent survival factors including age, sex, race, Charlson comorbidity score (CC), income, facility type, insurance, chemotherapy, sequence number, and year-of-diagnosis (Table 1B). Older patients were more likely to die compared to younger patients with age <55 (55≤age<65: HR=1.43, p<0.0001; 65≤age<75: HR=1.89, p<0.0001; and age≥75: HR=4.29, p<0.0001); male were more likely to die compared to female (HR=1.17, p<0.0001); blacks were more likely to die compared to white (HR=1.28, p<0.0001); patients with CC ≥1 had higher chance to suffer death compared to patients with CC =0 (HR=1.72, p<0.0001); patients at lower income area were more likely to die compared to patients at ≥$63,000 income area ($48,000 - $62,999: HR=1.16, p<0.0001; $38,000 - $47,999: HR=1.23, p<0.0001; and <$38,000: HR=1.30, p<0.0001); patients at other facility type were more likely to die compared to patients at Academic/Research program (HR=1.09, p=0.0019); and patients with other insurance were more likely to die compared to patients with private insurance (PI) with (HR=1.31, p<0.0001), patients with insurance unknown status were also more likely to pass away compared to patients with PI (HR=1.26, p=0.0207); there was no significant difference in survival between patients with multi-agent chemotherapy and with single/unknown agent (HR=1.02, p=0.6436), and patients without chemotherapy were less likely to die compared to patients with single/unknown agent (HR=0.83, p<0.0001); patients with sequence number of not-zero (defined as > 1 malignant sites) were more likely to die compared to patients with sequence number of zero (single malignant site) with (HR=1.19, p<0.0001). And finally, patients diagnosed between 2004 and 2010 were more likely to die compared to patients diagnosed between 2011 and 2017 (HR=1.25, P<0.0001). Kaplan-Meier estimate (Figure 1A) showed that OS rate at 1, 3, and 5 years were 88.0%, 76.3%, and 65.8%, respectively. Figure 1B shows that the OS was worse for those with co-morbidities as reflected by CC ≥1.
Conclusion: In this large real-world retrospective analysis, we demonstrate racial, demographics and socioeconomic differences impacting the outcomes of WM patients. Older WM patients, male sex, black race, higher CC and lower income were significantly associated with lower OS. Patients with access to PI and academic centers had better OS but those with non-PI and treated at non-academic centers had inferior OS. In terms of disease specific factors, WM patients with higher tumor burden (>1 malignant sites) and those needing therapy had worse OS compared to patients with lower tumor burden and those observed without therapy. Interestingly, patients diagnosed between 2011 and 2017 had superior OS compared to the patients diagnosed between 2004 and 2010 likely due to advancement in therapy over time. Cancer disparity data specific to WM are lacking and our study highlights the importance of socioeconomic, demographics and racial factors in the prognosis of patients with WM in addition to the standard disease and treatment specific prognostic variables. Since the social determinants of health can greatly impact outcomes in WM, improving access to high quality care could potentially help overcome the observed disparity in the outcomes.
Disclosures
Chaulagain:Sanofi Genzyme: Consultancy, Honoraria; Janssen Biotech: Consultancy, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal